There has been an increase in awareness about Postpartum Depression in recent years, and a growing awareness of Postpartum Anxiety, but women who experience Postpartum OCD often suffer silently and don’t talk about their experiences because their thoughts are often shrouded in shame and fear of harming their baby.
Postpartum Obsessional Compulsive Disorder (OCD) is a subset of postpartum anxiety disorders, and includes a range of intrusive thoughts and compulsions. Unlike general postpartum anxiety, which can manifest as pervasive worrying, postpartum OCD is characterized by obsessive repetitive, unwanted and often distressing thoughts, often accompanied by compulsions – repetitive behaviors that one feels the urge to perform in response to an obsessive thought.
Ninety-one percent of new moms report having scary, intrusive thoughts about harm to their baby or themselves sometimes, but studies about the prevalence of Postpartum OCD suggests that only between 1.7% to 7.0% of new moms have them to the extent it can be diagnosed as Postpartum OCD. These rates vary so much due to the limited studies that are available and also, because women tend not to talk about these types of symptoms for fear of judgement or that their child will be taken away from them, I think the actual rate of occurrence is much higher.
With Postpartum OCD, the intrusive thoughts can take on various forms, often revolving around a new mother’s ability to care for her child. Common themes include fears of accidentally harming the baby, images of the baby or oneself in dangerous, negative or even sexual situations, and there are often preoccupations with cleanliness and orderliness to the point of obsession. These thoughts are extremely at odds with a new mother’s true beliefs and are highly distressing but women are scared to let anyone know what is happening to them.
In my 25 years of working with new moms I have met so many women who are scared and ashamed about the intrusive thoughts they are having, not knowing that they are experiencing a treatable mental health condition, and it is not happening because they are a bad mother. I am passionate about bringing more awareness about this condition and this blog aims to provide a comprehensive understanding of postpartum OCD, including details on OCD symptoms, potential risk factors, and treatment options available.
Recognizing Postpartum OCD Symptoms
Postpartum OCD presents as a subtype of the better-known obsessive-compulsive disorder. As the name suggests, it specifically affects women during the postpartum period, which is the first 12 months following the birth of a child. Women suffering from this condition may experience debilitating obsessional thoughts, as well as compulsive behaviors stemming from these thoughts. The obsessions are most commonly centered around the infant’s well-being, along with an intense fear of unintentionally harming their child. These intrusive thoughts can be extremely distressing to the new mother, and they often lead to excessive worry, guilt, and shame.
Compulsive behaviors often accompany obsessions, as the mother tries to ease her anxiety and protect her child. These behaviors may include washing their hands excessively, checking the baby’s room or crib multiple times, or being overly cautious when handling the baby. These compulsions may provide temporary relief, but they ultimately contribute to a vicious cycle of anxiety and further obsessions.
Knowledge is essential when it comes to identifying the symptoms of postpartum obsessional compulsive disorder (OCD). The primary feature of this mental health condition is the presence of intrusive, unwelcome thoughts surrounding the newborn’s safety and well-being. These obsessions can manifest in various ways, such as constant worry over accidentally dropping the baby or even more disturbing thoughts, like fearing that one might intentionally cause harm to the infant. While it is essential to emphasize that these thoughts are irrational and not reflective of the new mother’s intentions, they can still cause significant distress and guilt.
Along with these obsessions, postpartum OCD often involves performing compulsive behaviors to alleviate the anxiety triggered by intrusive thoughts. These compulsions can take several forms, including but not limited to:
- Excessive handwashing or cleaning to prevent the baby from being exposed to germs or illnesses.
- Repeatedly checking on the baby’s safety, such as ensuring the crib is properly set up, or checking on the baby’s breathing multiple times throughout the night.
- Seeking constant reassurance from others that the baby is safe and well.
- Avoidance behaviors, such as refusing to be left alone with the baby or withdrawing from daily life and social interactions.
Risk Factors for Postpartum OCD
Identifying who may be at risk of developing postpartum OCD is not an exact science, as the condition can affect women of various backgrounds and lifestyles. However, certain factors can contribute to a woman’s likelihood of developing the disorder. Some of these risk factors may include a personal or family history of anxiety, depression, or OCD, as well as hormonal imbalances caused by the rapid shift in hormone levels after childbirth.
While any new mother can potentially develop postpartum OCD, there are specific risk factors that may increase the likelihood of the condition. Being aware of these factors can help both the mother and those around her recognize possible warning signs, and support the mother in seeking professional assistance. Key risk factors for postpartum OCD include:
- Personal or family history of mental health disorders: Women with a history of anxiety disorders or OCD, either themselves or within their family, may have a heightened risk for developing postpartum OCD.
- Hormonal changes: The postpartum period is characterized by rapid shifts in hormone levels, which can contribute to the development of mood and anxiety disorders, including OCD.
- Stressful life events: The presence of external stress factors, such as a traumatic childbirth experience or difficulties in managing new motherhood, can exacerbate the risk of postpartum OCD.
- Previous perinatal loss: Women who have experienced miscarriages, stillbirths, or other forms of perinatal loss in the past may be more prone to postpartum OCD due to the heightened anxieties surrounding their new baby’s well-being.
Treatment Options for Postpartum OCD
For women suffering from postpartum OCD, multiple treatment options are available to suit each individual’s specific needs. Choosing the right course of action often comes down to personal preferences and the severity of the disorder. Here are some common treatment options:
- Cognitive-Behavioral Therapy (CBT): This form of psychotherapy has proven highly effective in treating OCD, including postpartum OCD. CBT focuses on recognizing and challenging irrational thought patterns, allowing individuals to regain control of their fears and anxieties.
- Exposure and Response Prevention (ERP): A specialized CBT technique, ERP involves gradual and controlled exposure to anxiety-inducing thoughts or situations, while simultaneously resisting the urge to carry out compulsive behaviors.
- Medication: Depending on the severity of the disorder, medication, such as selective serotonin reuptake inhibitors (SSRIs), may be prescribed by a healthcare professional. Medication can be an effective way to manage the symptoms of postpartum OCD and can be used as part of a larger treatment plan that include therapy.
- Support groups: Connecting with other women experiencing similar difficulties can offer both emotional support and practical advice in dealing with postpartum OCD.
Resilience and Hope for the Future
Recovering from postpartum OCD may seem challenging at times, but it is essential to remember that hope and resilience can pave the way to a healthy future. With the right support, understanding the condition’s symptoms, risk factors, and treatment options, women suffering from postpartum OCD can regain control of their lives, build a strong bond with their newborn, and enjoy motherhood more. Postpartum obsessional compulsive disorder is a reality that many new mothers face, often silently. By shedding light on this mental health condition, increasing awareness, and providing support, we can play a crucial role in helping affected women seek the help and care they deserve. No mother should suffer in silence – please reach out if you or a loved one are experiencing symptoms of postpartum OCD.
No article would be complete without mentioning the best book I have ever read about Postpartum Scary Intrusive Thoughts. It is called Good Moms Have Scary Thoughts by Karen Klein. It is available from Amazon.

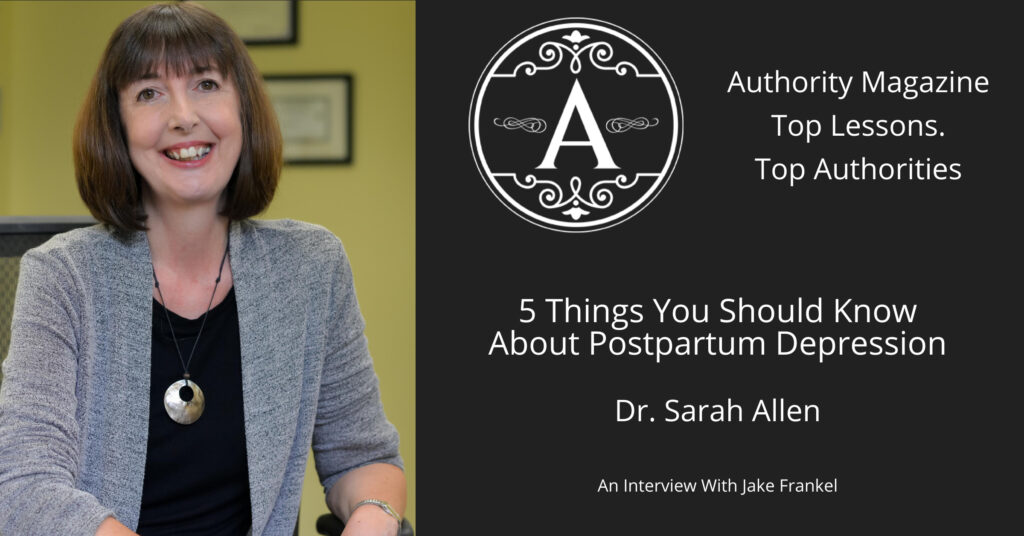
Dr. Sarah Allen has 25+ years of experience in private practice helping women to transition to being the mom they want to be. She is the Founding Director of the statewide non-profit Postpartum Depression Alliance of IL. She also specializes in pregnancy loss & infertility & has published research on postpartum depression and traumatic childbirth.
If you would like to work with Sarah, please phone her at 847 791-7722 or on the form below.
If you would like to read more about me and my areas of specialty, please visit Dr. Sarah Allen Bio. Dr. Allen’s professional license only allows her to work with clients who live in IL & FL & the UK and unfortunately does not allow her to give personalized advice via email to people who are not her clients.
Dr. Allen sees clients in person in her Northbrook, IL office or remotely via video or phone.
What Can I Read That Helps Me While I Am Waiting For My First Appointment With Sarah?
If you feel that you may be experiencing pregnancy or postpartum mood disorder, or worry that you may be at risk of developing it, please download my free booklets below.
See each specific webpage to download one or many.